Hemophilia and other bleeding disorders have long been recognised as conditions with significant medical implications. However, beyond the immediate health concerns, these disorders also impose a substantial economic burden on individuals, families, and society as a whole. Living with hemophilia often means grappling with not only the physical challenges but also the financial strain that comes with managing such a chronic condition. It’s not just about the cost of medicines but also about the long-term impact on quality of life, employment, and the psychological well-being of patients and their families.
Globally, millions of people are affected by hemophilia and bleeding disorders, with varying degrees of severity and impact. While modern medicine has made strides in managing these conditions, the cost associated with treatment remains a pressing concern. Patients often require lifelong treatment, regular medical consultations, and, in severe cases, emergency interventions. All these factors contribute to a financial challenge that can be overwhelming for many families, particularly those without adequate health insurance or access to government assistance.
Understanding the economic impact of hemophilia is crucial for policymakers, healthcare providers, and society at large. By shedding light on the financial aspects, we can work towards better support systems, improved access to affordable treatments, and ultimately, a better quality of life for those affected. This article delves into the complexities of the economic burden associated with hemophilia, exploring the direct and indirect costs, the role of healthcare systems, and potential strategies to alleviate these challenges.
What Are Hemophilia and Bleeding Disorders?
Definition and Types
Hemophilia is a rare genetic disorder that impairs the blood’s ability to clot. This can lead to excessive bleeding, both internally and externally, following an injury. The two most common types of hemophilia are Hemophilia A and Hemophilia B. Hemophilia A is caused by a deficiency in clotting factor VIII, while Hemophilia B results from a deficiency in factor IX. Both conditions are typically inherited, though they can also occur due to spontaneous genetic mutations.
In addition to hemophilia, there are other bleeding disorders, such as Von Willebrand Disease, which affects the blood’s ability to clot due to a deficiency or dysfunction of the Von Willebrand factor. While less severe than hemophilia, Von Willebrand Disease is the most common hereditary bleeding disorder and can also have significant health and economic impacts.
Causes and Symptoms
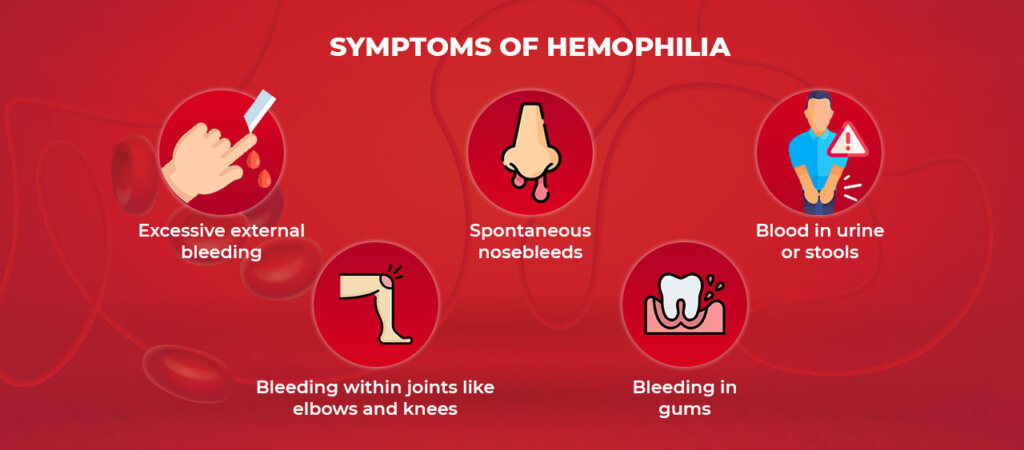
Hemophilia is primarily a genetic disorder passed down through families, often affecting males more frequently than females due to its linkage to the X chromosome. The symptoms of hemophilia and other bleeding disorders can vary widely, depending on the severity of the condition. Common symptoms include prolonged bleeding from cuts or injuries, spontaneous bleeding into joints or muscles, excessive bruising, and, in severe cases, life-threatening hemorrhages.
For individuals with bleeding disorders, even minor injuries can result in prolonged bleeding, leading to additional medical intervention and treatment, further compounding the economic burden.
The Global Prevalence of Hemophilia
Statistics and Figures
Hemophilia is a rare disorder, with an estimated prevalence of about 1 in 10,000 births for Hemophilia A and 1 in 30,000 for Hemophilia B. Although it affects a relatively small percentage of the population, the impact is significant due to the high cost of treatment and care. According to the World Federation of Hemophilia, there are over 400,000 individuals living with hemophilia worldwide.
Regions with the highest rates of hemophilia often face challenges related to treatment availability and healthcare infrastructure. In developed countries, advanced treatment options are available, albeit at a high cost. In contrast, developing nations may struggle with limited access to necessary medical interventions, exacerbating the condition’s impact.
Challenges in Data Collection
Various factors, including underdiagnosis, misdiagnosis, and lack of access to healthcare facilities in many parts of the world complicate accurate data collection on hemophilia prevalence. Furthermore, social stigma and lack of awareness can contribute to hesitancy in seeking medical attention, resulting in incomplete data and challenges in resource allocation.
Economic Impact on Individuals and Families
Medical Costs
One of the most significant economic burdens of hemophilia is the cost of treatment. The primary treatment for hemophilia involves replacing the missing clotting factor, which can be extremely expensive. Factor replacement therapy, whether through prophylactic (preventative) treatment or on-demand (as needed) therapy, requires regular and often lifelong administration, contributing to substantial healthcare costs.
In addition to factor replacement therapy, individuals with hemophilia may require other medical interventions, such as surgery or physiotherapy, to manage complications resulting from joint damage due to repeated bleeding episodes. The cumulative cost of medical care, including hospital stays, emergency room visits, and medications, can be overwhelming for many families.
Indirect Costs
Beyond the direct medical expenses, hemophilia also imposes indirect economic burdens. For many patients and their families, the condition can lead to loss of income due to the inability to work regularly. Parents may need to take time off work to care for affected children, further exacerbating financial strain. In addition, the emotional and psychological impact of living with a chronic condition can affect mental health and overall quality of life.
For families without comprehensive health insurance or financial support, the economic impact can be devastating, leading to difficult choices between medical care and other essential needs.
Healthcare System and Societal Costs
Healthcare Expenditure
The financial burden of hemophilia extends beyond individual patients to healthcare systems. Treating bleeding disorders requires significant resources, including specialized healthcare professionals, medical facilities, and treatment supplies. In countries with national healthcare systems, the cost of hemophilia care can consume a substantial portion of the healthcare budget, prompting discussions about cost-effectiveness and resource allocation.
Social Implications
Hemophilia and other bleeding disorders also carry social implications, affecting patients’ ability to participate fully in society. Stigma and discrimination can lead to social isolation and hinder educational and employment opportunities. Support from community organizations and advocacy groups is crucial in combating these challenges, but such support often requires financial resources that may be scarce.
Treatment and Management Costs
Types of Treatments
Treatment for hemophilia has evolved significantly over the years, with several options available depending on the severity of the condition. Prophylactic treatment, where clotting factor is administered regularly to prevent bleeding episodes, is considered the gold standard for severe hemophilia. However, the high cost of clotting factor concentrates can be prohibitive.
On-demand treatment, administered during or after a bleeding episode, may be more cost-effective in the short term but can lead to long-term complications and increased healthcare costs. Innovative therapies, such as extended half-life products and non-factor replacement therapies, offer promising alternatives but are often accompanied by high price tags.
Access to Treatment
Access to treatment remains a significant barrier for many individuals with hemophilia, particularly in low- and middle-income countries. Disparities in treatment availability and affordability can lead to inadequate care and poor health outcomes. Health insurance plays a crucial role in providing access to necessary treatments, but coverage can be inconsistent, leaving many patients vulnerable to financial hardship.
Policy and Funding for Hemophilia
Government Initiatives
Governments around the world play a crucial role in supporting individuals with hemophilia through national health policies and funding for research and treatment. Policies that ensure access to affordable healthcare, support early diagnosis and promote awareness are essential in reducing the economic burden of hemophilia.
Role of Non-Governmental Organizations
Non-governmental organizations (NGOs) and international bodies are instrumental in supporting hemophilia patients, particularly in regions with limited resources. These organizations provide funding for treatment, advocate for policy changes, and offer education and support services. Case studies of successful interventions by NGOs highlight the importance of collaboration and resource-sharing in addressing the economic challenges of hemophilia.
Innovations and Research in Treatment
Recent Advances
Recent advances in hemophilia treatment have focused on improving patient outcomes and reducing the economic burden. Gene therapy, which aims to correct the underlying genetic defect, holds promise for a potential cure but is still in the experimental stages and may be costly to implement.
New medications, such as bispecific antibodies and small interfering RNA (siRNA) therapies, offer novel approaches to managing hemophilia and may prove to be cost-effective in the long run by reducing the frequency of bleeding episodes and improving quality of life.
Future Prospects
The future of hemophilia treatment is promising, with ongoing research into innovative therapies and improved delivery methods. As these treatments become more widely available, they have the potential to significantly reduce the economic burden of hemophilia by decreasing the need for frequent medical interventions and improving patients’ overall health and well-being.

Reducing the Economic Burden
Strategies for Cost Reduction
Reducing the economic burden of hemophilia requires a multifaceted approach that includes effective management strategies, early diagnosis, and education campaigns. Encouraging adherence to treatment regimens and promoting healthy lifestyles can help prevent complications and reduce healthcare costs.
Community Support and Advocacy
Community support and advocacy are essential in addressing the economic challenges faced by individuals with hemophilia. Building strong networks of patients, families, healthcare providers, and advocacy groups can foster a supportive environment that encourages patient self-advocacy and empowers individuals to take control of their health.
Conclusion
The economic burden of hemophilia and bleeding disorders is a complex issue that requires comprehensive strategies and collaboration among healthcare providers, policymakers, and the community. By understanding the financial challenges faced by individuals and families, we can work towards better support systems, improved access to affordable treatments, and ultimately, a better quality of life for those affected. It is crucial to continue investing in research and innovation to find more cost-effective solutions and ensure that all individuals with hemophilia have the opportunity to lead fulfilling lives.
FAQs?
What is the primary cause of hemophilia?
Hemophilia is primarily caused by genetic mutations that affect the blood’s ability to clot. It is often inherited, with mutations occurring in the genes responsible for producing clotting factors.
How does hemophilia affect daily life?
Hemophilia can significantly impact daily life, as individuals must be cautious to avoid injuries that could lead to excessive bleeding. Regular treatment and medical appointments are often necessary, which can disrupt work and social activities.
What are the most common treatments for hemophilia?
The most common treatments for hemophilia include factor replacement therapy, which involves infusions of the missing clotting factor, and newer therapies such as bispecific antibodies and gene therapy.
Why are bleeding disorders expensive to manage?
Bleeding disorders are expensive to manage due to the high cost of medications, frequent medical interventions, and the need for specialized healthcare services. Long-term management often requires ongoing treatment and monitoring.
How can families cope with the financial strain?
Families can cope with the financial strain by seeking support from healthcare providers, advocacy groups, and government programs that offer assistance and resources. Planning and budgeting for medical expenses can also help manage costs.
What role do governments play in supporting patients?
Governments support patients by implementing national health policies, providing funding for research and treatment, and ensuring access to affordable healthcare. Policies that promote awareness and early diagnosis are also crucial.
Are there any promising treatments on the horizon?
Promising treatments on the horizon include gene therapy, which aims to correct the underlying genetic defect, and new medications such as siRNA therapies that offer novel approaches to managing hemophilia. These treatments have the potential to improve patient outcomes and reduce costs in the long term.