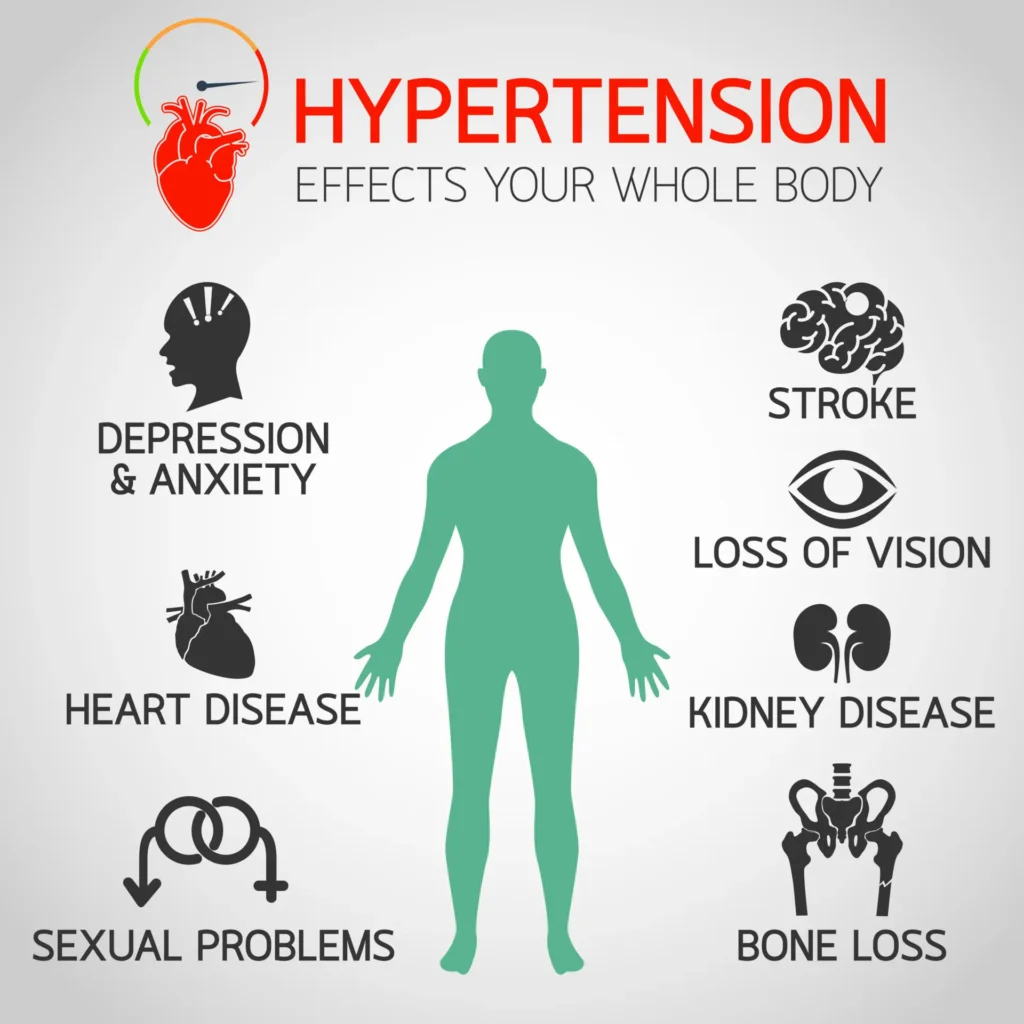
Hypertension, often dubbed the “silent killer,” is a prevalent health condition affecting millions of people worldwide. It’s a condition that quietly sneaks up on you, often without noticeable symptoms, yet it can lead to severe health complications like heart disease, stroke, and kidney failure if left unchecked. Managing hypertension involves a combination of medications and lifestyle changes, each with its associated costs. Understanding these costs is crucial for patients, healthcare providers, and policymakers alike as they navigate the complexities of treatment options and financial considerations. This article aims to delve into the intricate web of hypertension management costs, exploring both the medical expenses related to medications and the potential financial implications of lifestyle modifications.
Hypertension, or high blood pressure, is not just a health issue; it’s a significant financial concern that affects individuals and healthcare systems globally. With healthcare costs rising and the economic burden of chronic diseases increasing, understanding the cost-effectiveness of hypertension treatments has never been more important. This article will explore the different facets of treating hypertension, providing insights into medication costs, lifestyle changes, and how these two approaches compare in terms of financial impact and long-term health benefits.
Understanding Hypertension
What is Hypertension?
Hypertension is a chronic medical condition where the blood pressure in the arteries is persistently elevated. Blood pressure is measured in millimetres of mercury (mmHg) and is recorded as two numbers: systolic (the pressure in your blood vessels when your heart beats) and diastolic (the pressure when your heart rests between beats). A typical reading is around 120/80 mmHg. When these numbers rise consistently above 140/90 mmHg, a person is considered to have hypertension. This condition forces the heart to work harder to pump blood, leading to potential damage to the heart, blood vessels, and other organs over time.
Causes and Risk Factors
The exact cause of hypertension often remains elusive, but several risk factors contribute to its development. These include genetics, age, obesity, sedentary lifestyle, excessive salt intake, and excessive alcohol consumption. Chronic conditions like diabetes and kidney disease can also increase the risk. Stress and poor dietary habits further exacerbate the situation, making lifestyle management a critical component of hypertension treatment.
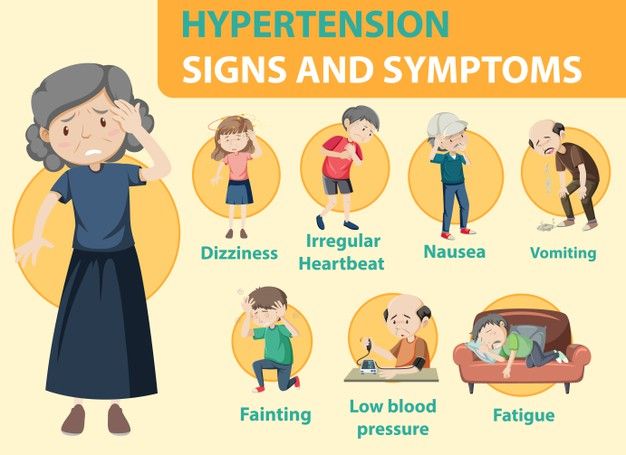
Symptoms and Diagnosis
One of the challenging aspects of hypertension is its often asymptomatic nature. Many individuals may not experience noticeable symptoms until the condition has progressed significantly. Common symptoms, when they occur, might include headaches, shortness of breath, dizziness, or nosebleeds, but these are not specific to hypertension and can result from other issues as well. Diagnosis typically involves regular blood pressure monitoring and may include additional tests to assess organ function and identify any underlying conditions.
The Financial Burden of Hypertension
Direct Costs: Medical Expenses
The direct costs of managing hypertension include doctor visits, diagnostic tests, and medications. For many, this means regular consultations with healthcare providers, often leading to frequent tests to monitor the condition’s progression and adjust treatment plans accordingly. These recurring medical expenses can add up quickly, particularly for those without comprehensive insurance coverage.
Indirect Costs: Lost Productivity and Quality of Life
Beyond direct medical expenses, hypertension incurs indirect costs that can be equally significant. These include lost productivity due to health-related absences, reduced work capacity, and diminished quality of life. Chronic hypertension can lead to fatigue, cognitive decline, and increased vulnerability to other health complications, all contributing to a broader economic impact on individuals and society.
Medications for Hypertension
Types of Medications
Hypertension is often treated with a variety of medications, each targeting different aspects of blood pressure control. The choice of medication depends on individual patient needs, existing health conditions, and potential side effects.
- ACE Inhibitors: These medications help relax blood vessels by blocking the formation of a natural chemical that narrows blood vessels. Common examples include enalapril and lisinopril.
- Beta-Blockers: These work by reducing the workload on the heart and opening up blood vessels, causing the heart to beat more slowly and with less force. Examples include atenolol and metoprolol.
- Calcium Channel Blockers: These prevent calcium from entering the heart and blood vessel cells, leading to lower blood pressure. Amlodipine and diltiazem are commonly prescribed.
- Diuretics: Often referred to as “water pills,” diuretics help the kidneys remove excess sodium and water, reducing blood volume and pressure. Hydrochlorothiazide is a typical example.
Cost of Medications
The cost of hypertension medications varies widely, influenced by factors such as the type of drug, whether it is branded or generic, and the patient’s insurance coverage. Generic medications are typically less expensive than their branded counterparts, offering a cost-effective solution for many patients. However, even with insurance, out-of-pocket expenses can be significant, particularly for those on multiple medications.
- Generic vs. Branded Medications: Generic drugs offer the same effectiveness as branded ones at a lower cost, making them an attractive option for cost-conscious patients. The price difference can be substantial, and opting for generics can lead to significant savings over time.
- Insurance Coverage and Out-of-Pocket Expenses: Insurance coverage can greatly influence medication costs, with policies varying in terms of co-pays, deductibles, and the range of covered medications. Understanding one’s insurance benefits and exploring generic options are essential steps in managing these costs effectively.
Lifestyle Changes for Hypertension Management
Dietary Modifications
Dietary changes play a pivotal role in managing hypertension, offering a non-pharmacological approach that can complement or even reduce the need for medications.
- The DASH Diet: The Dietary Approaches to Stop Hypertension (DASH) diet is specifically designed to combat high blood pressure. It emphasises fruits, vegetables, whole grains, lean proteins, and low-fat dairy while reducing saturated fats and cholesterol. Following the DASH diet has been shown to lower blood pressure significantly.
- Reducing Salt Intake: Excessive salt consumption is a known contributor to hypertension. Reducing salt intake by avoiding processed foods and using herbs and spices for flavouring can have a profound impact on blood pressure levels.
Exercise and Physical Activity
Regular physical activity is another cornerstone of hypertension management. Engaging in activities like walking, jogging, swimming, or cycling for at least 150 minutes a week can help lower blood pressure, improve cardiovascular health, and contribute to weight loss, all of which are beneficial in managing hypertension.
Stress Management Techniques
Chronic stress is a significant contributor to hypertension. Techniques such as meditation, yoga, deep breathing exercises, and mindfulness can help reduce stress levels, indirectly contributing to better blood pressure control. Investing time in stress management can also improve overall mental health and quality of life.
Cost Implications of Lifestyle Changes
While lifestyle changes often involve upfront costs—such as gym memberships, dietary supplements, or wellness programs—they can lead to long-term savings by reducing the need for medications and medical interventions. Moreover, investing in a healthy lifestyle often results in improved overall well-being, which can have positive ripple effects on productivity and quality of life.
Comparing Costs: Medications vs. Lifestyle Changes
Short-term and Long-term Cost Analysis
In the short term, medications might seem more convenient and cost-effective due to their immediate impact on blood pressure levels. However, the long-term costs associated with chronic medication use can be substantial, especially when considering potential side effects and the risk of medication dependency.
Lifestyle changes, while requiring more effort and discipline, offer sustainable and cost-effective solutions. Over time, adopting healthy habits can lead to reduced medication needs and lower healthcare costs. Furthermore, lifestyle changes address the root causes of hypertension, providing a holistic approach to health management.
Effectiveness and Sustainability
The effectiveness of hypertension management strategies varies among individuals, and a combination of medications and lifestyle changes often yields the best results. Medications can provide quick relief and are essential for severe cases, but lifestyle modifications offer lasting benefits that address underlying risk factors. The sustainability of lifestyle changes, however, depends on an individual’s commitment and access to resources like healthy food options and exercise facilities.
The Role of Preventive Measures
Regular Health Screenings
Regular health screenings are a vital component of hypertension prevention and management. Early detection through routine blood pressure checks allows for timely intervention, reducing the risk of complications and associated costs. Many healthcare providers offer free or low-cost screenings, making this a cost-effective preventive measure.
Community and Workplace Interventions
Community-based programs and workplace wellness initiatives can play a significant role in preventing and managing hypertension. These interventions often include health education, fitness programs, and stress reduction workshops, providing valuable resources for individuals to make positive lifestyle changes. Such programs not only benefit individual health but also contribute to reduced healthcare costs and improved productivity at the community level.
Challenges in Managing Hypertension Costs
Economic Disparities
Economic disparities can significantly impact an individual’s ability to manage hypertension effectively. Those with limited financial resources may struggle to afford medications, healthy foods, or access to exercise facilities. Addressing these disparities requires a multi-faceted approach involving policy changes, community support, and increased access to affordable healthcare services.
Access to Healthcare Services
Access to healthcare services remains a critical challenge in managing hypertension costs. Rural areas, in particular, may face shortages of healthcare providers, making it difficult for residents to receive timely diagnosis and treatment. Telemedicine and digital health tools offer promising solutions to bridge these gaps, providing remote access to healthcare consultations and monitoring.
Future Trends in Hypertension Treatment Costs
Innovations in Medications and Treatments
Advancements in medical research are leading to the development of new hypertension treatments, potentially offering more effective and affordable options in the future. Innovations such as personalised medicine, which tailors treatment plans to an individual’s genetic makeup, hold promise for improving treatment outcomes while optimising costs.
Telemedicine and Digital Health Tools
The rise of telemedicine and digital health tools is transforming hypertension management by providing convenient and cost-effective solutions for monitoring and treatment. Mobile apps and wearable devices allow patients to track their blood pressure, receive personalised recommendations, and communicate with healthcare providers remotely. These technologies not only enhance patient engagement but also reduce the need for in-person visits, lowering overall healthcare costs.
Conclusion
Managing hypertension effectively requires a comprehensive approach that balances the costs and benefits of medications and lifestyle changes. While medications offer immediate relief and are essential for many patients, lifestyle modifications provide sustainable and long-term solutions that address the root causes of hypertension. By investing in preventive measures, improving access to healthcare services, and leveraging technological advancements, we can reduce the financial burden of hypertension and enhance overall health outcomes.
Ultimately, the key to managing hypertension costs lies in empowering individuals with the knowledge, resources, and support they need to make informed decisions about their health. By fostering a culture of health and wellness, we can mitigate the impact of hypertension on individuals and society, paving the way for a healthier and more financially sustainable future.
FAQs?
What is the most cost-effective medication for hypertension?
The most cost-effective medication for hypertension often depends on individual patient needs and insurance coverage. Generic medications, such as generic versions of ACE inhibitors, beta-blockers, and diuretics, are typically more affordable than branded ones while offering similar efficacy.
How can I reduce my hypertension treatment costs?
To reduce hypertension treatment costs, consider opting for generic medications, exploring insurance benefits, and incorporating lifestyle changes like a healthy diet and regular exercise. Preventive measures, such as regular health screenings, can also help detect hypertension early and reduce long-term costs.
Are lifestyle changes enough to control hypertension without medication?
For some individuals with mild hypertension, lifestyle changes may be sufficient to control blood pressure levels. However, those with more severe hypertension or additional risk factors often require a combination of medications and lifestyle modifications for effective management.
What are the hidden costs of hypertension treatment?
Hidden costs of hypertension treatment can include lost productivity due to health-related absences, diminished quality of life, and potential side effects of medications that may require additional treatments. These indirect costs can significantly impact individuals and society.
How does insurance affect hypertension treatment costs?
Insurance coverage can greatly influence hypertension treatment costs, affecting co-pays, deductibles, and out-of-pocket expenses. Understanding your insurance benefits and opting for covered medications and services can help manage these costs effectively.
What are the long-term financial benefits of managing hypertension effectively?
Managing hypertension effectively can lead to long-term financial benefits by reducing the risk of complications like heart disease and stroke, decreasing the need for costly medical interventions, and improving overall quality of life and productivity.
Can digital health tools help reduce the cost of hypertension treatment?
Yes, digital health tools, such as mobile apps and wearable devices, can help reduce hypertension treatment costs by providing remote monitoring, personalised recommendations, and convenient communication with healthcare providers. These tools enhance patient engagement and reduce the need for in-person visits, lowering overall healthcare expenses.